1. Introduction
In Somerset, we want people to live healthy and independent lives, supported by thriving and connected communities, with timely and easy access to high quality and efficient support when they need it.
This Policy sets out the overarching principles and key processes that enable the Local Authority (Somerset Council) and NHS Somerset’s Integrated Care Board (ICB) to ensure the care provision offered to our residents is of the highest quality.
We define this as services that provide excellent care, tailored to the needs of each individual they support. There is an expectation that all regulated services that operate within Somerset are either outstanding or good with the Care Quality Commission. Any provider that is unable to adhere to a good rating will be supported in ways outlined within this Policy.
Both organisations are committed to working with all regulated and non-regulated adult social care providers to share best practice, identify potential quality issues at an early stage, and collectively work to improve quality standards. By doing so, we seek to reduce the risk of business failure and ultimately ensure that people in Somerset are receiving good and outstanding care. This work is also underpinned by our contractual responsibilities in relation to the contract management and oversight of commissioned services and is the statutory duties set out within the Care Act 2014.
We recognise the vital and valuable contribution of our local care market and workforce and seek to support a transparent and productive working relationship between our organisations and all those services supporting people within the local community.
We will follow the following principles in our contract compliance and quality assurance activity to help improve the quality of adult social care and encourage our providers to do the same:
- Promote quality through everything that we do
- Champion quality as a central principle, demonstrating that it should, and can be, maintained and improved alongside financial sustainability
- Provide clarity and consistency by promoting a shared view of quality
- Listen to, involve and act on the views of people who use services and their families and carers. We will understand and monitor their views of the quality of services
- Promote a person-centred approach which treats all people with respect, compassion and dignity in a caring environment
- Promote people’s human rights and their rights to equality with others
- Support and encourage improvement
- Listen to the views of care staff to understand how we can better support them
- Use our combined intelligence to highlight and act on emerging issues and guide and share best practice
- Identify and provide advice on the principles for improving quality and focus our efforts where the need for improvement is greatest
- Promote reliability so that people who use services have confidence in the support they receive
- Coordinate action
- Offer advice, develop guidance and provide forums to resolve issues.
By following these principles and encouraging others to do the same, we will promote high quality, person-centred care and support services to enable those using services to say:
- “I feel in control and safe.”
- “I have the information I need when I need it.”
- “I have access to a range of support that helps me live my life.”
- “I am in control of my support, in my own way.”
- “I have considerate support delivered by competent staff.”
- “I can decide the kind of support I need.”
This is a working document and will be revised as required and reviewed, at a minimum, annually via the joint Care Provider Commissioning and Quality Board. The Policy will be updated in line with any changes the regulator makes to its framework, or to reflect legislative or organisational changes and developments.
To inform my organisation’s work, and improve quality and safety, we use CQC’s definition of quality and safety. The definition of quality is set out in CQC’s assessment frameworks, and is based on the NHS National Quality Board shared single view of quality and the Quality Matters definition of quality.
2. Statutory Duties, Powers and Responsibilities
The Local Authority has a number of commissioning responsibilities under the Care Act 2014 that are of relevance to this policy:
The duty to promote diversity and quality in service provision:
The Care Act statutory guidance states that ‘high quality, personalised care and support can only be achieved where there is a vibrant, responsive market of services available’. The Local Authority role is seen as critical and under section 5 of the Care Act, has a duty to shape and maintain an efficient and effective market of services for meeting care and support needs in the local area.
The duty applies in relation to services that the Local Authority commissions directly, but also to other non-commissioned services in its area (including those used by self-funders), universal services and services provided by partners (such as health or charitable services) that together create the marketplace.
The market that is shaped should ensure that any person requiring Care and Support/Support services:
a. Has a variety of providers supplying a variety of services to choose from;
b. Has a variety of high quality services to choose from; and
c. Has sufficient information to make an informed decision about how to meet the needs in question.
In order to fulfil its duty to promote diversity and quality in service provision the Local Authority must ensure it has effective strategies to shape the marketplace and commission the right services.
Market shaping and commissioning of adult care and support services
Market shaping involves engaging with stakeholders to understand the current local supply and demand for services and predict or anticipate what the future needs are likely to be based upon the changing needs and aspirations of people who use services. There is an expectation in the Care Act that the Local Authority will carry out market shaping activity in collaboration with relevant partners, including people who have Care and Support needs and carers.
Commissioning: Commissioning is the Local Authority activity of determining at a strategic level which of the Care and Support/Support services in the marketplace it should design, deliver, monitor and evaluate itself through a contractual arrangement and which it should not.
Procurement: Procurement is the specific function of buying or acquiring a service (or services) and agreeing how that service will be delivered. Some services will likely be procured in advance, so they are available when required and others will be procured as and when it is deemed appropriate to do so (for example, a specialist service to meet a particular person’s complex needs).
Contracting: Contracting is the means by which the procurement process becomes legally binding. Contract management then ensures that the services (or services) continue to be delivered according to the standards agreed.
Recommissioning: Recommissioning is the process of reviewing then renewing a contractual arrangement with a provider.
Decommissioning: Decommissioning is the process by which the Local Authority withdraws from a contractual arrangement with a provider.
The Local Authority also has a duty to promote the Wellbeing of people with Care and Support needs and carers with Support needs in everything it does, including market shaping and commissioning activity. For further detail please see The Duty to Promote Individual Wellbeing.
The Local Authority must also understand the outcomes that are most important to people living in its area and demonstrate that these outcomes are at the heart of local commissioning strategies and policies.
To support the Local Authority to fulfil its duty to promote individual Wellbeing and outcomes in everything it does the Care Act statutory guidance recommends that outcomes-based commissioning is considered. Outcomes based commissioning means developing service arrangements that are based on the provider being able to support the person, carer or local population to achieve a set of agreed outcomes relating to Wellbeing alongside the meeting of eligible Care and Support needs.
Managing Provider Failure
This section of the Care Act applies to regulated Care and Support provision only. It does not apply for non-regulated social care activity provision. Regulated provision includes:
a. Personal care
b. Care home provision for people requiring personal care or nursing care
c. Care home provision for people requiring treatment for substance abuse
d. Treatment of disease, disorder (including learning disability) or injury; and
e. Assessment or treatment of people detained under the Mental Health Act 1983.
If a service provider providing regulated Care and Support activities in a Local Authority area becomes no longer able to do so then the Local Authority has a temporary duty under section 48 of the Care Act to meet the needs of affected persons or carers. The duty applies for as long as it appears necessary to do so.
The duty to temporarily meet needs only applies when the business has failed and is not able to continue providing the service. It does not apply when there is an alternative arrangement in place to continue the provision of services (e.g. where the business is taken over by an administrator).
This duty applies from the time that the Local Authority becomes aware that the provider’s business has failed[1].
This temporary duty to meet needs applies regardless of whether:
- The person or carer is ordinarily resident in its area (or even the same country of the UK);
- The person or carer is known to the Local Authority;
- The provider is known to or has a contractual arrangement with the Local Authority;
- The person makes their own Care and Support arrangements (either through a Direct Payment or is self-funding);
- The services were arranged by a different Local Authority;
- The Local Authority has carried out a needs or carers assessment;
- The Local Authority has carried out a financial assessment; or
- The needs apparent are eligible under the National Eligibility Criteria.
Managing other service interruptions
This section applies where either:
- There is temporary interruption to any Care and Support service (Regulated and Non-Regulated); or
- A provider of a non-regulated Care and Support activity fails.
Service interruptions happen for a number of reasons, for example:
- Illness affecting a substantial number of the workforce meaning the service is temporarily unavailable or reduced (e.g. home care provision);
- Illness affecting people with Care and Support needs meaning that a service is temporarily unavailable (e.g. a Norovirus breakout in a Day Service); or
- Business challenges facing an organisation meaning that some services may be temporarily unavailable.
Under section 19 of the Care Act the Local Authority has the power to meet any need that it considers urgent, regardless of factors such as whether an assessment has been completed or whether the person is ordinarily resident in its area.
When services are interrupted or a non-regulated activity is no longer available the statutory guidance is clear that the Local Authority should consider exercising this power if the service provider is not able to identify a solution, if the level of risk is high or if the situation is likely to deteriorate into something unsustainable without the Local Authority becoming involved.
The Local Authority has a separate Business Failure policy and supporting checklist to ensure the care and support needs of service users continue to be met in the event of a business failure. The contract monitoring and quality assurance activity outlined within this Policy helps identify early warning of potential failure.
Safeguarding
Safeguarding means protecting an adult’s right to live in safety, free from abuse and neglect. It is about people and organisations working together to prevent and stop both the risks and experience of abuse or neglect, whilst at the same time making sure that the adult’s wellbeing is promoted including, where appropriate, having regard to their views, wishes, feelings and beliefs in deciding on any action.
Safeguarding adults is everyone’s business. The safeguarding duties under The Care Act 2014 apply to an adult who:
- Has needs for care and support (whether or not the local authority or NHS Somerset is meeting any of those needs) and;
- Is experiencing, or is at risk of abuse or neglect; and
- As a result of those care and support needs is unable to protect themselves from either the risk of or the experience of abuse or neglect.
The Care Act 2014 set out a clear legal framework for how local authorities and other parts of the system should protect adults at risk of abuse or neglect.
Local authorities have a number of safeguarding duties. They must:
- lead a multi-agency local adult safeguarding system that seeks to prevent abuse and neglect and stop it quickly when it happens
- make enquiries, or request others to make them, when they think an adult with care and support needs may be at risk of abuse or neglect and they need to find out what action may be needed
- establish Safeguarding Adults Boards, including the local authority, NHS and police, which will develop, share and implement a joint safeguarding strategy
- carry out Safeguarding Adults Reviews when someone with care and support needs dies as a result of neglect or abuse and there is a concern that the local authority or its partners could have done more to protect them
- arrange for an independent advocate to represent and support a person who is the subject of a safeguarding enquiry or review, if required.
Any relevant person or organisation must provide information to Safeguarding Adults Boards as requested.
There may be individuals who receive services from any provider from which the Locality Authority or NHS Somerset commissions services for whom safeguarding concerns have been identified and/or will require a statutory (section 42) enquiry to support their safety and wellbeing.
Staff working in settings where people receive commissioned care will actively participate in any statutory safeguarding enquiry requirement under section 42 of The Care Act (2014), staff will also participate in any non-statutory safeguarding enquiry when appropriate. Staff will also, where appropriate, contribute to any safeguarding meetings and the development and implementation of any safeguarding plans.
Both the Local Authority and NHS Somerset follows Somerset’s Multi Agency Safeguarding Adults Policy and it is the expectation that all providers of care within Somerset area follow the guidance for safeguarding adults in Somerset via: Policy and Procedure – Somerset Safeguarding Adults Board (safeguardingsomerset.org.uk)
[1] A full list of all the reasons that a regulated business can be deemed to be subject to business failure can be found in The Care and Support (Business Failure) Regulations 2015
3. The role of the Care Quality Commission (CQC)
As the independent regulator of health and adult social care, the CQC has the overarching role to monitor, inspect and regulate health and social care services to make sure those who use these services receive high-quality, safe, effective and compassionate care.
In July 2022, the CQC launched their new single assessmet framework built on their five key questions and well-known ratings system, and is what the regulator uses to set out its view of quality and make judgements. The framework not only applies to providers, but also to Local Authorities and Integrated Care Systems since April 2023.
Visit – Our new single assessment framework – Care Quality Commission (cqc.org.uk)
The CQC is able to take enforcement action against registered persons who breach conditions of registration and/or relevant sections of legislation. They can also take enforcement action against unregistered providers providing regulated activities.
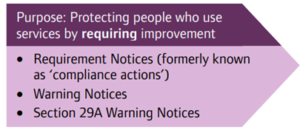
The CQC has two primary purposes when using enforcement powers:
- to protect people who use regulated services from harm, and the risk of harm, and to ensure they receive health and social care services of an appropriate standard by either requiring or forcing improvement; and
- to hold providers and individuals to account for failures in how the service is provided
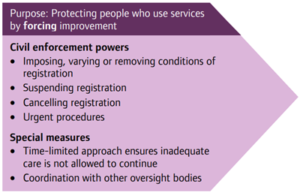
The CQC can use different types of civil enforcement action in order to achieve these purposes including imposing, removing or varying conditions of registration; cancelling registration; urgent procedures; and special measures:
The Local Authority and NHS Somerset ICB both work closely with the CQC as part of routine system surveillance activity.
However, the role and remit of our local Quality Assurance functions is not to replicate that of a regulator. It is in our collective best interest to have services in Somerset that meet the needs of our citizens, and that thrive and succeed. Through our monitoring and assurance functions, we will support and work alongside our local care providers in obtaining the best possible standards of care, as well as holding them accountable for doing so. We are well placed to offer and secure good quality advice, guidance and information from partners across our local health and care system in order to achieve this aim.
4. Provider Quality Governance and Oversight arrangements
Within Somerset, the Local Authority and NHS Somerset ICB have a number of key forums and functions where issues relating to provider quality, risk and performance are monitored and overseen.
Of particular note:
- Joint Care Provider Commissioning & Quality Board: The purpose of this Board is to support clearer evidence-based commissioning/de-commissioning decision-making relative to the ongoing quality and safeguarding concerns in our care market. The Board is also responsible for reviewing this Policy on at least an annual basis to ensure it remains accurate and relevant. The Commissioning and Quality Board has a remit to determine further action to be taken following non-compliance with an agreed rectification action plan; this includes issuing Rectification Notices, Final Warning Notices or letters of termination to de-commission a service. It meets on a quarterly basis and also reviews the ‘state of the Somerset Care Market’ using data and local intelligence to support oversight.
- Somerset System Quality Group (SQG): SQGs are intended to support the effective delivery of the quality component of the ICS (Integrated Care System) Strategy through the coming together of partners around these common priorities and active signals and concerns, developing system responses to shared concerns, testing new ideas that can make a difference, reflecting and learning. This is chaired by NHS Somerset ICB.
5. Our Quality Assurance Approach in Somerset
The services we commission should promote safety, wellbeing, independence, a good quality of life, be person-centred and contribute to the individual outcomes desired by those using the service. It is expected that commissioned care will meet people’s health and social care needs holistically.
We expect all care providers to meet the CQC’s fundamental standards: The fundamental standards | Care Quality Commission (cqc.org.uk)
For regulated services in Somerset, the minimum quality standard is a ‘Good’ CQC rating both overall and in all five key domains: The five key questions we ask | Care Quality Commission (cqc.org.uk)
For unregulated services in Somerset we expect the same minimum quality standard of Good overseen through the providers’ completion of Service Assessment Forms (SAFs) which are returned and analysed by the Contract Manager and given a RAG rating. These are supported through contract and/or quality visits.
With regards to Somerset’s growing Micro-Provider market, in order to be registered as a ‘trusted provider’ on the Somerset Community Connect Directory each provider has provided evidence that they meet the ‘doing it right’ quality standards of the Somerset Micro-enterprise Programme. This includes:
- DBS Checks
- Public Liability Insurance
- Terms of Service
- Support Plan
- Complaints and Safeguarding Policy
The programme also offers a quality feedback loop which means that any providers or who do not share a commitment to the ‘Doing it right’ Quality Standard will be removed from the programme.
How we monitor quality and risk across Care Provision in Somerset
We monitor quality and risk in a variety of ways:
a) Quality Assurance Framework (QAF)
As set out in Section 2, Local authorities have a requirement to meet their statutory duties under the Care Act 2014 and together with NHS partners, we are committed to supporting measurable improvements in Provider quality and maintain effective market insight & analysis of market quality.
PAMMS: The PAMMS tool was originally co-produced with Providers when the South East Regional Local Authorities came together to produce a tool for use that would enable them to consistently measure quality, spend and activity within commissioned services. It is now recognized nationally as a good practice tool, used across many regions and large numbers of local authorities. During 2022/23 the South West region piloted the PAMMS QA module (a digital tool enabling local authorities and providers to gather information to meet quality standards consistently) with volunteer providers and working in partnership with provider representatives to prepare for formal adoption.
While PAMMS is a relatively new digital system for us, it is not new activity – LAs had already long undertaken quality assurance activity. What PAMMS helps to offer is better consistency of approaches regionally so we can fulfil our duties as commissioners for safe and effective market assurance in a way that is not arduous for providers and can be managed within our resources availability to achieve better outcomes for the people who receive care and support. It providers an online portal for assessment feedback & co-produced action planning, and helps improve care service quality. reduces multiple QA assessments & action plans, reduce the impacts of provider failure and enhance local, sub-regional, regional & national collaboration.
PAMMS Quality Assurance Module Since April 2023, the PAMMS QA Module has been adoptted for all our Quality Assurance visits in Somerset. There are six sections in which to assess the provider’s quality – Standards are assessed in all appropriate areas in order to ‘triangulate’ the evidence:
- Assessment, Care Planning & Reviews
- Service User’s Experience
- Care Worker Knowledge & Understanding
- Staff Training & Recruitment
- Environment, Equipment & General Safety
- Leadership, Quality Assurance & Management
Provider Quarterly Returns: Care providers contracting with either the Local Authority or NHS Somerset are required to complete a quarterly quality assurance return on the Pamms portal. The return consists of a questionnaire with Key Performance Indictors ( KPIs) embedded. Multi-agency meetings are convened quarterly to review submissions with the aim of identifying whether any system support is needed or can be offered to help address falling or consistently low KPI results. The routine monitoring of quality and risk align with our contractual and statutory duties.
We encourage providers to use the dashboard as an external review of the quality of care being delivered and as a benchmark with providers offering similar services in Somerset.
This information can be shared by either the provider or the commissioner with the regulator to triangulate information about the quality of care in Somerset services
We will utilise the following process and approach to address any non-compliance with the quarterly return process with Registered Managers:
b) CQC Inspection reports and ratings
We routinely monitor latest CQC Inspection ratings and reports and use overall ratings to inform provider’s overall RAG score[1]
NHS Somerset ICB and the Local Authority maintain regular contact with the CQC, and some provider intelligence may also be shared through these engagements.
Our contracts require providers to notify us of any outcome following compliance assessments by the CQC, and to work with us to develop an improvement plan to action the identified areas for improvement within the agreed timescales. Residents / clients should also be informed as part of the improvement plan.
c) Service Quality Feedback (SQF) information
Our SQF forms enables us to monitor and consider feedback from a variety of sources, including health and care professionals, people who use local services, their relatives, visitors, the wider public, and independent organisations (such as Healthwatch Somerset) to monitor quality.
We expect quality issues to be resolved as part of routine care management processes at a local level. We would expect that concerns or complaints are raised with the Manager of the provider service in the first instance. There will be occasions where individuals are not satisfied with the provider response and further investigation is required by our teams. People can also tell us about gaps in our services. Information is very important as it tells us how useful the service is, how good the care is and where there may be problems or things that could be improved.
Where we receive significant numbers of SQFs highlighting concerns – or patterns of concern – this may reduce the RAG rating. Isolated feedback will not usually alter the score; however this will depend on the nature and severity of the report.
d) Financial risk
Where provision falls into a market risk category (see below), providers will be asked to provide the Local Authority with its most recent audited accounts on an annual basis. If we identify financial concerns or have concerns relating to business sustainability, we may also require you to submit your most recent audited accounts. Financial returns will be assessed by the Council’s finance officers and risk scored. A medium or high risk score could trigger a discussion with the Local Authority’s Commercial and Procurement Team.
e) Other intelligence
Information is also gathered from professional teams accessing commissioned services. This may include feedback from Social Care workers, care sourcing or brokerage teams, CHC and FNC Assessment staff, LARCH team staff, Safeguarding professionals or Quality Assurance personnel, whistle-blowers, Somerset Partnership NHS Foundation Trust staff, District Nurses, Community Psychiatric Nurses, GPs, Primary Link, Primary Care Networks and other authorities who commission and provide services in Somerset.
The Somerset Safeguarding Adults Board has published a service monitoring checklist setting out examples of potential indicators for concern within provider settings. The areas of care listed may highlight that care is neglectful and could be harmful to residents, and is of use to professionals working across health and care: https://ssab.safeguardingsomerset.org.uk/wp-content/uploads/SSAB-Service-Monitoring-Checklist-v2.3.pdf
[1] Please note, if you have a CQC overall rating that is “Good” but there are some areas ‘Requiring Improvement’, we will contact you to discuss these areas in more detail.
6. Our Quality Improvement Activity
Whilst the responsibility for providing consistently good quality care lies with care providers themselves, ‘Commissioners have a responsibility to assure themselves of the quality and safety of the organisations they place contracts with[1]’.
This policy will be invoked where a provider is identified as not meeting quality standards.
Where serious, repetitive and/or several quality concerns are received or detected by the Local Authority and/or NHS Somerset ICB, an unannounced Quality Visit will take place.
During these visits, spot checks will be made in relation to all operational practices. Discussions will be had with residents/service users, relatives, and staff, with preliminary feedback provided to the Registered Manager prior to a report being provided outlining findings and any improvements required.
NHS Somerset ICB may contact the provider via telephone in the first instance to advise and issue a contract performance notice in accordance with the NHS Care Service Contract.
The Local Authority will contact the provider to advise that the Quality Improvement process outlined within this policy is being implemented and to arrange a meeting to discuss the areas of concern at a timeline in line with the outcomes of any investigations; in the case of nursing care (where residents are CHC funded), this will include representatives from NHS Somerset ICB.
Quality Improvement Management (QIM) Meetings will include the Home Manager and a senior manager from within the organisation. The purpose is to discuss the areas of concern and to apply the necessary actions to improve the quality of care. Follow up QIM meetings are arranged according to progress being made. The QIM will be closed when the Home is considered to have achieved a good quality standard by NHS Somerset and/or the Local Authority; as part of this approach, there is an expectation that the Nominated Individual will attend the QIM given the responsibilities of this position.
Both commissioning organisations have the right to independently or collectively suspend commissioning services from the provider until such time that minimum standards are met. This decision will be proportionate to the assessed level of presenting risk in relation to quality and/or safeguarding. Both organisations will continue to work with and support the provider to reach (and aim to exceed) acceptable minimum expectations.
With the permission of the provider, we will also (where appropriate) engage with other support organisations or functions (for example the Registered Care Providers Association, LARCH Collaboration Team, IPC or Public Health team) to provide additional proportionate assistance to the quality issues identified.
The provider will be asked to produce an improvement plan identifying the tasks to be undertaken (unless the areas of concern are already being addressed within an improvement plan agreed with the CQC). They should allocate responsibilities for action and clear timescales for completion, and review progress on the plan on a routine basis. The timescale will be set to reflect the nature of the concern. Decisions will be taken on any further action required following review.
Depending on the nature of the concern, and given the need to be transparent, the Local Authority may also write to all provider service users and their families to advise them of what is happening, or arrange a joint Health and Social Care meeting with them. This will ensure everyone receives consistent and accurate information, and that any anxieties are appropriately managed. This will be done in partnership with the provider. NHS Somerset may contact in person, or via telephone, any person using the service. Where people lack capacity to make decisions about their care, NHS Somerset will contact the family, representative or IMCA service to advise of concerns and seek their feedback about the service.
The Local Authority will inform colleagues in host and placing authorities of provision placed under QIM, the nature of the concerns and invite attendance at QIM meetings. QIM meeting minutes will be shared with all placing authorities. Communication threads will be maintained, where necessary, to ensure matters arising outside of QIM meetings are shared. Likewise, the reverse happens where people placed in provisions in other LA areas that are under quality improvement measures in support of best practice guidance for out of area placements and commissioning.
Where standards continue to remain below Policy/CQC expectations, and/or where the provider fails to engage with us, sustain improvements, or where there are repeat episodes of quality/safety concerns, the provider will be referred to the Joint Commissioning and Quality Board. The Board can issue a Rectification Notice or Final Warning Notice and has the decision making authority to suspend (or continue to suspend) commissioning from the provider until such time that minimum quality standards are met. The Board also has the right to terminate contracting arrangements with the provider if quality standards are consistently not met or improvements fail to be sustained as evidenced by the CQC, Quality Assurance and/or safeguarding outcomes.
Where there are serious/numerous concerns giving rise to immediate/continued Quality and/or Safeguarding intervention, we reserve the right to apply sanctions outside of the Quality Improvement Process. This decision will be taken at Quality Assurance Service Manager or above.
In the event of a contract termination, arrangements will be made to meet with the provider to discuss the breach of contract and next steps. The Board also has a responsibility to respond to CQC intervention or regulatory action of providers (28 days notice) to ensure the health and wellbeing risk of residents/services users is maintained; the needs of people using the service will always remain paramount. All users of the service/family will be written to, to explain the situation, what we will do and how we will support them. We will make every effort to ensure that individuals remain in control, and have choice about the care and support they receive. Best interest meetings (including with relevant family members and/or friends, advocates, and professionals) will be held for those unable to make decisions about changing services (e.g. moving to a different provider) as a consequence of services no longer being commissioned. Service users and/or the key people in their lives will be supported to find alternative service provision. An exception will be agreed for anyone who chooses to continue receiving care and support from the provider, as long as the provider remains CQC registered and that the person fully understands what this means.
Where there are significant concerns about quality and/or safeguarding and the commissioning position has been changed to reflect this, the name of provider will be included in a Managed Placements Memo to make staff aware when considering placements. This will only be implemented following discussion with the provider at a Quality Improvement Meeting or Provider Safeguarding Meeting unless there are exceptional circumstances. Placements may be restricted in full or in part as part of this approach. Providers themselves also have the right to manage placements into their provision to enable them to address any improvements that may be required.
Only specifically designated Council managers and NHS Somerset ICB senior managers can authorise a change of commissioning status in relation to their respective organisations.
The Managed Placements Memo is shared between Local Authority and Health staff involved in supporting people to find care and support in the community and in care services. Staff will first contact the named manager on the Memo, before making contact with that provider, so that they can be fully aware of the issues and to enable them to discuss them with the people making choices about the providers they use, and/or their families where appropriate. When the quality and/or safeguarding issue(s) have been resolved the designated manager will ask for the provider details to be removed from the list immediately, which will then be re-issued.
[1] https://www.gov.uk/guidance/care-and-support-statutory-guidance/safeguarding
7. Meet the Teams
Our Teams include staff with considerable professional experience of working with and for health and care services and working successfully with service providers and managers to identify and plan improvements to the quality of their service.
Somerset Council’s Care Provider QA Team
Adult Social Care QA Team Structure

Kelly Senior – Service Manager, Care Provider Quality Assurance

Christine Hale – Quality Assurance Officer (Home Care, Home Care closures and/or service transfers)

Natasha Gosney – Quality Assurance Officer (Supported Living, Micro-providers and Supported Living Service Transfers)

Nikki Burgess – Quality Assurance Officer (Nursing and Residential Care Homes and closures – East of the county)

Sian Angel – Quality Assurance Officer (Nursing and Residential Care Homes and Closures, West of the county)

Sarajane Willis – Quality Assurance Officer (LD Residential, Closures and Day Care)
Our Local Authority ASC Quality Assurance staff are supported to undertake training and CPD in relation to quality improvement. Staff are also supported to complete the Care Certificate Framework The Care Certificate Standards (skillsforcare.org.uk), an identified set of standards that health and social care workers adhere to in their daily working life and equips workers with the fundamental skills they need to provider quality care. Our staff understand how regulatory compliance works in practice and what is required to achieve a ‘good’ or ‘outstanding’ Care Quality Commission rating.
NHS Somerset ICB CHC and Care Sector Quality Team

Clare Woodhead – Continuing Healthcare Quality (CHC) and Care Sector Manager

Penny Knight – CHC and Care Sector Quality Assurance Nurse

Natalie Ledlie – CHC and Care Sector Quality Assurance Nurse

Amanda Jaggers – CHC and Care Sector Quality Assurance Nurse
The Continuing Healthcare Quality Assurance team work jointly with Providers, Council colleagues, NHS partners, CQC and wider organisations to promote the development and maintenance of high standards of care and where people are at the heart of our work . The team are encouraged to develop through training and collaboration with specialists and providers so that they can share learning and good practice with all Somerset Providers.
Feedback and contact
Care Provider feedback is really important to both the Local Authority and NHS Somerset ICB, and is crucial in helping us to deliver the best possible support to our local care market.
We will be proactive in seeking feedback following any Quality Improvement activity or business failure intervention. but encourage feedback at any time about your experience of the service we provide via our Feedback Form:
Care Provider Quality Assurance Feedback Form
You can also reach our team via email – ascproviderqualityassurance@somerset.gov.uk
